Summary
Description
Juxtacortical chondroma (synonym: periosteal chondroma) is a rare benign surface lesion composed of cartilage.
People and Age
Children as young as 7 as well as adults may present with this rare lesion in the foot.
Symptoms and Presentation
The lesion presents with pain and swelling.
Brief description of the xray
Radiographically the lesion has its epicenter in the region of the outer cortical surface of the bone.
Brief desc of tx
Treatment is by curettage or marginal resection, depending on location.
Tumor Name
Tumor Type
Benign or Malignant
Body region
Most Common Bones
Location in bone
Periosteal reaction
Position within the bone
Tumor behavior
Tumor density
Complete Information on this Tumor
Introduction and Definition
Juxtacortical chondroma (synonym: periosteal chondroma) is a rare benign surface lesion composed of cartilage. It is similar in appearance and location to periosteal osteosarcoma. The potential for confusion with periosteal and even parosteal osteosarcoma mandates a thorough investigation and biopsy of these lesions.
Incidence and Demographics
Children as young as 7 as well as adults may present with this rare lesion in the foot.
Symptoms and Presentation
The lesion presents with pain and swelling.
X-Ray Appearance and Advanced Imaging Findings
Radiographically the lesion has its epicenter in the region of the outer cortical surface of the bone. There is no stalk or peduncle as in an osteochondroma. The most common location is adjacent to the metaphysis. The cortex may be involved to a variable degree, but the lesions do not involve the medullary space. There is a mass outside the confines of the bone that contains cartilage and amorphous ossification.
In the cases of this lesion I have seen there were no ring and arc figures seen in the ossified matrix, and neither was there any trace of trabecular organization of the ossified material.
There is no periosteal reaction, but the lesion may lift the periosteum and create "columns" or "buttresses" of mature periosteum at each end of the mass that appear to project out from the axis of the bone. Pressure from growth of the lesion may create a saucer shaped or complex shaped defect in the underlying bone.
Bone scan will show that the lesion is actively making bone, and is only helpful to count lesions.
CT scan shows a more precise picture of the lesion and its juxtacortical location. It may reveal the amorphous character of the ossific material within the lesion, as well as help in distinguishing the tumor from osteochondroma, osteoid osteoma, and myositis ossificans, but not from periosteal osteosarcoma and parosteal osteosarcoma. CT should be done even if an MRI has been done.
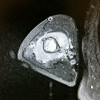
MRI will provide more information about the extent of the lesion, but will not be adequate to identify the lesion or to rule out a malignancy. The MRI may help identify the cartilage component. The MRI images of the case shown here demonstrate a markedly lobular appearance of the tumor.
To differential the lesion from the surface osteosarcomas, look for a mass of very heavily ossified tumor bone plastered in the surface of the bone. Periosteal osetosarcoma tends to be more diaphyseal, a little less ossified, and has a more rapid growth pattern as compared to juxtacortical chondroma. I myself would not feel confident making a call of juxtacortical chondroma based on imaging alone, most cases will require a careful biopsy, making sure the lesion is fully sampled.
In the cases of this lesion I have seen there were no ring and arc figures seen in the ossified matrix, and neither was there any trace of trabecular organization of the ossified material.
There is no periosteal reaction, but the lesion may lift the periosteum and create "columns" or "buttresses" of mature periosteum at each end of the mass that appear to project out from the axis of the bone. Pressure from growth of the lesion may create a saucer shaped or complex shaped defect in the underlying bone.
Bone scan will show that the lesion is actively making bone, and is only helpful to count lesions.
CT scan shows a more precise picture of the lesion and its juxtacortical location. It may reveal the amorphous character of the ossific material within the lesion, as well as help in distinguishing the tumor from osteochondroma, osteoid osteoma, and myositis ossificans, but not from periosteal osteosarcoma and parosteal osteosarcoma. CT should be done even if an MRI has been done.
MRI will provide more information about the extent of the lesion, but will not be adequate to identify the lesion or to rule out a malignancy. The MRI may help identify the cartilage component. The MRI images of the case shown here demonstrate a markedly lobular appearance of the tumor.
To differential the lesion from the surface osteosarcomas, look for a mass of very heavily ossified tumor bone plastered in the surface of the bone. Periosteal osetosarcoma tends to be more diaphyseal, a little less ossified, and has a more rapid growth pattern as compared to juxtacortical chondroma. I myself would not feel confident making a call of juxtacortical chondroma based on imaging alone, most cases will require a careful biopsy, making sure the lesion is fully sampled.
Laboratory Findings
Laboratory exam will help only in confirming that there is no systemic condition such as infection.
Histopathology findings
On gross pathology, the lesion consists of cartilage and ossified cartilage. On microscopic exam there is benign cartilage with typical chondrocytes in scattered lacunae and noneoplastic bone being formed by enchondral ossification. There is no neoplastic cartilage with hypercellularity or bizarre chondrocytes, and no neoplastic osteoid or bone as in periosteal osteosarcoma.
Treatment Options for this Tumor
Treatment is by curettage or marginal resection, depending on location.
Outcomes of Treatment and Prognosis
Recurrence is uncommon.