Case ID Number
Image Types
Image modality
Tumor Name
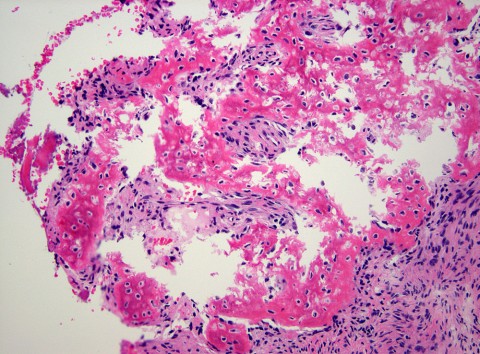
Example Image
yes
Tumor Type
Benign or Malignant
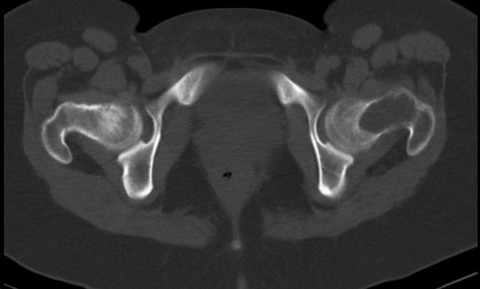
Body region
Bone name
Location in the bone
position within the bone