Summary
Giant cell tumor of tendon sheath is a rare, solitary benign soft tissue tumor which may arise in the tendon sheath tissues of the hand and wrist as well as the ankle and foot. Most cases occur in the hand, where local recurrence after excision has been reported in up to 40% of cases. Approximately 3 - 10% of these tumors occur in the foot, most commonly in the forefoot, especially the great toe. ((Ushijima) Most patients are young adults, around age 30.
Clinically, the patients report a slow growing painless, firm solitary mass adjacent to the dorsal or plantar tendons, the midfoot joints, or the ankle joint, which has been present for one to two years on average. There may be a history of trauma, and neurological symptoms occur rarely. In one study, lesions in the forefoot occurred in the first, second, and fifth rays exclusively, indicating that there may be some relationship between weight-bearing and this tumor. The tumor may cause or accentuate an angular deformity such as hallux valgus.
Complete Information on this Tumor
CT scan will show the extent of the tumor, and clearly delineate any bony involvement. Some of these tumors have small calcifications, feature shared with synovial sarcoma.
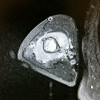
MRI scans are helpful to define the extent of the lesion, and can be helpful in the preoperative diagnosis. Hemosiderin in the lesion may result in vary low signal intensities on some sequences, and the lesions enhance on T1 sequences after administration of gadopentetate contrast agent, and these features help identify the tumor.
Histologically, the lesion is similar to pigmented villonodular synovitis. There is hemosiderin and frequent macrophages, foam cells, and giant multi-nucleated cells. The origin of the tumor is unclear. DNA aneuploidy, chromosomal translocations, and tumor expression of p63 and nm23 have been reported in a variable proportion of cases. Expression of p63, has been identified in giant cell tumor of bone, pigmented villonodular synovitis, and the giant cell tumor of tendon sheath, leading to speculation that these may share a common origin. The giant cells in all 3 of these tumors have been found to demonstrate features that are associated with osteoclast, including tartrate- resistant acid phosphatase marking, and calcitonin receptor expression.