There is no doubt about the value of an accurate and timely determination of fracture risk. Treatments for the prevention of fracture are more cost effective and lead to vastly better outcomes.
Surgeons should be able to relatively easily enumerate the factors that influence the fracture risk of any particular patient. They should attempt to estimate the cost/benefit ratio of the surgical treatment required. Finally, they should use the Mirel's system to assign a fracture risk score. The decision for or against surgery should be based on a combination of the Mirel's score and the clinical judgement of the surgeon.
RECOMMENDATIONS
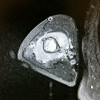
There is no doubt about the importance of determining which cancer patients with metastatic bone disease have had enough damage to their bones to increase their risk of developing a fracture. Prophylactic fixation of these patients clearly decreases morbidity in patients compared to fixation of completed fractures. The difficulty lies in determining a good set of criteria that allows surgeons to accurately determine the patient population requiring prophylactic fixation. Many different criteria have been suggested including the size of the lesion; the type of cancer that metastasized to bone; the location of the metastatic lesion; pain due to the lesion; whether the lesion is lytic or blastic; irradiation of the lesion; and the use of biomechanics to predict fracture.
However researchers have disagreed on which are the important features to use for diagnosis of imminent fractures as in most cases there has been evidence published that supports and that refutes the use of each of the features for diagnosis. When deciding which criteria to use, it is important to consider both the accuracy with which it predicts an increased risk for fracture and the convenience with which it can be measured. The biomechanical factors that Hipp proposes to use seem as though they would be good predictors of fracture, but Hipp did not provide an easy way to collect the data required making them less useful as a diagnostic tool. While there is evidence that the size of the lesion could be a good predictor for fracture, the difficulty in accurately determining the size radiographically makes it less useful diagnostically.
The other variables discussed are much easier to determine in patients and therefore would seem more useful diagnostically. However, based on the research it seems that one criteria alone is not accurate enough to predict and increased risk of fracture. Rather, having the requirement for fixation involve the presence of several of these criteria would be better because while each criteria individually is subject to error by the physician, probability indicates that the chance of having false negatives and false positives would decrease with the more factors involved. Therefore, this writer feels that, while not ideal, the best diagnostic system to use is the scoring system proposed by Mirels who requires the analysis of 4 criteria in determining risk of fracture. In addition, his research indicates specific scores over which patients should have prophylactic surgery.
Therefore, surgeons would be able to relatively easily determine which of the criteria their patient has, assign them a score, and decide whether to perform surgery based on the score and clinical suspicion. While this system seems to be the best for now, it is likely that with improvements in imaging studies and further research, new criteria and modifications of old criteria will soon be proposed. . Metastatic bone disease is the most common malignant bone lesion seen in adults. Bone is the third most common site for metastases after the lung and the liver (H,I). 7-27% of all cancer patients each year are likely to have a metastatic bone defect (H). The incidence of pathologic fractures in patients with malignant disease is 1-2% and 25% of all metastases to long bones progress to fractures